Learn More about the Next Meeting

What is COPD?
COPD IS:
Chronic "long term"
Obstructive "blockage to air flow"
Pulmonary "The Lungs"
Disease "Illness, or a sick condition"
COPD is a chronic condition which will progressively reduce air flow into the lungs unless treated. Usually this condition is diagnosed after deterioration of lung capacity has already occurred. Though there are treatments that can combat the continued progress of this ailment, a return to full lung capacity is not possible. An increased shortness of breath is the ongoing trait of COPD, and must be immediately treated in order to prevent further deterioration.
COPD is also called: chronic obstructive lung disease (COLD), chronic obstructive airway disease (COAD), chronic airflow limitation (CAL) and chronic obstructive respiratory disease (CORD).
Symptoms of COPD
- Dyspnea: Loss of breath during normal activities
- Decreasing exercise tolerance
- Wheezing
- Chronic coughing
- Increasing phlegm (mucus) production
- "Smokers cough" each morning
- Colds and flu last longer than previously experienced
- Repeating respiratory infections
- Bronchitis each winter
- Unable to keep pace with people from your same age group
Do not excuse these symptoms as being the result of being "out of shape," allergies, or because you are often near other people who are ill. Fast treatment for COPD is the best chances for slowing and preserving lung capacity.
What causes COPD?
The number one cause of COPD is tobacco use, with an estimate of 80-90% of cases directly attributable to cigarette smoking and other tobacco uses.1
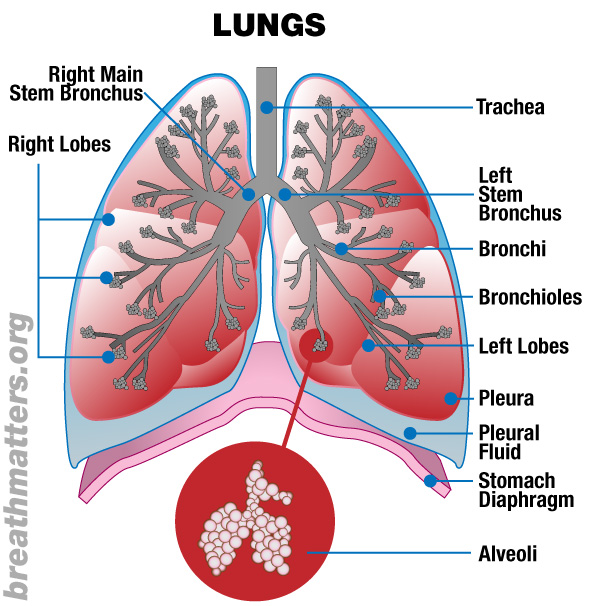
COPD is caused by poisonous particles of gas that triggers an abnormal inflammatory response in the lung. The inflammation created by this reaction brings on chronic bronchitis. In the alveoli, this inflammatory response causes destruction of the tissues of the lung, an ongoing process known as emphysema.
Diagram of Human Lungs
Avoiding infections
Protecting yourself from illness is the best defence when you have COPD. Colds, flu, viruses cause lung disease to worsen.
The U.S. News and World Report web site has some very good tips on staying well while dealing with COPD:
Talk with your doctor about vaccines. Most COPD patients should get the flu shot each year in the fall. You also should get a pneumonia vaccine every five to seven years. Neither of these vaccines guarantees that you won't get these illnesses, but they greatly reduce your risk.
Wash your hands frequently, especially during flu season. When you use an ATM machine, for instance, or open doors or turn on faucets, germs can collect on your hands. If you then rub your eyes or nose or touch your mouth, the germs can enter your body, making you sick. When washing hands, use soap and warm water, work up a good lather, and wash for 30 seconds, about as long as it takes to say the alphabet.
Avoid crowds, and don't socialize with people who are sick. If your friend has a cold, don't get too close, or consider rescheduling until he or she has recovered and is no longer infectious.
COPD and Sleep
The U. S. News and World Report article had a plethora of helpful information, an example is this tip about sleeping and COPD:
Our brains are designed to protect us and keep us alive. Deep in our brain is a region that constantly samples our blood to be sure that we are getting enough oxygen and breathing clean, healthful air. If it detects anything wrong, it sends out an alarm that feels to us like a sudden rush of anxiety or panic. This feeling prods us into getting up and away from whatever is interfering with our breathing.
With COPD, you regularly have trouble breathing, and your suffocation alarm can become hyperactive. As a result, you may feel edgy or anxious a lot of the time or feel panicky at being hurried or when you smell strong odors.
It is important to understand that this is common in people with COPD and that you aren't falling apart emotionally or mentally. With help from your doctor, there are a number of things you can do to "reset" your suffocation alarm. These include:
- Breathing training
- Counseling and relaxation training
- Anti-anxiety medications
Footnotes:
1. Medicinenet.com, information accessed May 2011


